 This CE activity was originally published in The Rx Consultant. If you received credit for it previously, you cannot receive credit for it again.
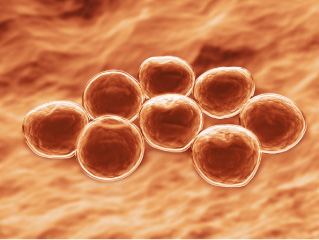
This CE activity was originally published in The Rx Consultant. If you received credit for it previously, you cannot receive credit for it again.Staphylococcus aureus is a leading cause of infection in both the community and hospital settings. A highly virulent and hardy pathogen, it is notable for its ability to cause a wide variety of infections, ranging from simple skin and soft tissue infections (SSTIs) to life-threatening infections such as osteomyelitis and sepsis. Staphylococcus aureus is broadly subdivided into methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant Staphylococcus aureus (MRSA). A common misconception among both clinicians and the general public is that MRSA causes more severe infections than MSSA. In reality, both organisms cause the same general types of infections, including life-threatening infections. However, from a drug therapy perspective, MRSA manifests a higher degree of antimicrobial resistance than MSSA, making treatment a challenge in both the outpatient and inpatient settings.
For many years, MRSA was considered a nosocomial pathogen, primarily encountered in large, tertiary healthcare institutions. However, over the last 2 decades, there has been a dramatic increase in the incidence of MRSA infections in community and outpatient settings. Infections originating in these settings are commonly called community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) infections; those originating in the hospital or other healthcare settings (eg, skilled nursing facilities) are generally termed healthcare-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) infections. This issue will review important concepts related to MRSA infections, with a focus on CA-MRSA. Important management strategies, including new antibiotics used in the treatment of MRSA, will be highlighted. With the increasing incidence of CA-MRSA infections, as well as a global increase in antimicrobial resistance in this pathogen, community providers play an important role in educating both patients and other providers about appropriate treatment options.
For many years, MRSA was considered a nosocomial pathogen, primarily encountered in large, tertiary healthcare institutions. However, over the last 2 decades, there has been a dramatic increase in the incidence of MRSA infections in community and outpatient settings. Infections originating in these settings are commonly called community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) infections; those originating in the hospital or other healthcare settings (eg, skilled nursing facilities) are generally termed healthcare-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) infections. This issue will review important concepts related to MRSA infections, with a focus on CA-MRSA. Important management strategies, including new antibiotics used in the treatment of MRSA, will be highlighted. With the increasing incidence of CA-MRSA infections, as well as a global increase in antimicrobial resistance in this pathogen, community providers play an important role in educating both patients and other providers about appropriate treatment options.
Format
This CE activity is a monograph (PDF file).
Fee
$10.00
CE Hours
1.50
CE Units
0.150
Activity Type
- Knowledge-based
Target Audience(s)
- Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, and Registered Nurses
Accreditation(s)
This CE activity was developed by The Rx Consultant, a publication of Continuing Education Network, Inc.
CE activities for Pharmacists and Pharmacy Technicians:
This continuing education (CE) activity meets the requirements of all state boards of pharmacy for approved continuing education hours. CE credit is automatically reported to CPE Monitor.
CE activities for Nurse Practitioners and Clinical Nurse Specialists:
This continuing education activity meets the requirements of:
The American Nurses Credentialing Center (ANCC) for formally approved continuing education (CE) hours, and CE hours of pharmacotherapeutics.
The American Academy of Nurse Practitioners Certification Program (AANPCP) for acceptable, accredited CE.
The American Nurses Credentialing Center (ANCC) for formally approved continuing education (CE) hours, and CE hours of pharmacotherapeutics.
The American Academy of Nurse Practitioners Certification Program (AANPCP) for acceptable, accredited CE.
This is a pharmacotherapeutics/pharmacology CE activity.
- The ANCC requires all advanced practice nursing certificants (CNSs and NPs) to complete 25 CE hours of pharmacotherapeutics as a portion of the required 75 continuing education hours.
- Pharmacology CE is recommended by the AANPCP and will be required for Certificants renewing certification starting January 2017.
- Most State Boards of Nursing require a minimum number of pharmacy contact hours to renew an advanced practice license.

Continuing Education Network, Inc. is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
Requirements for CE Credit
CE No Longer Valid
Pharmacists and Pharmacy Technicians -
Be sure your profile has been updated with your NAPB e-profile # and birth date information BEFORE completing the online evaluation, or your credits cannot be reported to CPE Monitor.
Continuing pharmacy education credit is automatically reported to CPE Monitor once the post-test & evaluation are successfully completed.
Objectives
- Identify specific factors that give Staphylococcus aureus high pathogenicity and relate these factors to treatment options.
- Describe the differences between CA-MRSA and HA-MRSA and the risk factors associated with each.
- List the oral and IV antibiotics used for the treatment of MRSA infections, and identify situations when their use is appropriate or inappropriate.
- Counsel patients on the potential adverse effects of the antibiotics for MRSA infections; discuss monitoring requirements and identify potential drug interactions.
Speaker(s)/Author(s)
|
Spencer H. Durham, Pharm.D., BCPS (AQ-ID) Brief Bio : Dr. Durham is an Assistant Clinical Professor at the Auburn University Harrison School of Pharmacy, Auburn, Alabama. He precepts 4th year Doctor of Pharmacy students during their Advanced Practice Experiences, and maintains a practice site at the Central Alabama Veterans Health Care System where he specializes in the field of infectious diseases. He also teaches in various courses throughout the pharmacy school and is active in several state and national organizations. In 2012, he was awarded an Added Qualification in Infectious Diseases by the Board of Pharmacy Specialties. Disclosure : Dr Durham reports no financial or personal relationship with any commercial interest producing, marketing, reselling, or distributing a product or service that appears in this issue. |
Activity Number
0428-0000-15-001-H01-P
Release Date:
Jan 20, 2015
Credit Expiration Date:
Jan 20, 2018
CE Hours
1.50
Fee
$10.00
